An individual with a dairy or milk allergy struggles with a potentially deadly food allergy. Specifically, this allergy causes overreactions in a person’s immune system upon interactions with proteins in milk or other milk products. Although cow milk is the most common type of allergy, sheep and goat milk can also be problematic.
Symptoms and Risk Factors
Ultimately, individuals of all age groups can develop a milk allergy, however, children younger than 16 are most impacted. Still, many of these young individuals tend to outgrow the condition. In the U.S., nearly 2% of children have developed a milk allergy, however, babies with intolerance to milk proteins usually overcome symptoms. Furthermore, both breastfed and formula-fed babies are likely to develop a milk allergy.
Generally, people can exhibit various systems that typically appear minutes or hours after consuming milk. However, immediate symptoms include wheezing, swelling, itching, vomiting, breathing difficulties, coughing, and hives. In contrast, a person can experience delayed symptoms such as diarrhea, watery eyes, loose stools, runny nose, and abdominal cramps.
For babies, in particular, a milk allergy can give them colic. Other common symptoms an individual can exhibit are skin rashes and digestive issues. However, remember that symptoms differ in people depending on onset and severity. This means some individuals may exhibit immediate symptoms, while others have delayed reactions.
Undetermined Causes
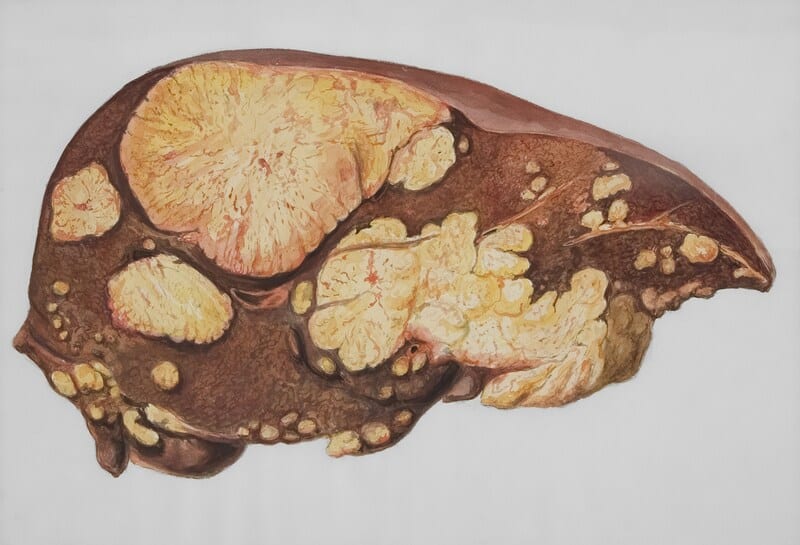
Currently, healthcare providers and researchers have yet to determine why a milk allergy develops so quickly. However, they’ve determined that two milk products cause the immune system to overreact: casein and whey. Particularly, casein makes up 80% of the protein in milk and can be found in yogurt, cheese, and solidified milk. Comparatively, the remaining 20% of milk protein is whey and makes up the liquid portion. Nonetheless, an individual can become allergic to both proteins or just one. Fortunately, having a milk allergy doesn’t make one contagious so passing the condition on to another isn’t a concern.
IgE Antibodies
However, they’ve discovered that a milk allergy occurs by triggering allergic reactions. Following milk consumption, an individual’s body produces immunoglobulin E (IgE) antibodies that stick to mast cells. From there, these antibodies encounter the milk proteins and release histamine, causing symptoms. Due to these rapid IgE reactions, a milk allergy risks becoming a potentially fatal condition known as anaphylaxis.
Conversely, non-IgE reactions gradually develop within 48 hours and occur mostly in babies. Typically, milk triggers non-IgE reactions, leading to intolerance to milk protein that isn’t life-threatening. Another difference with non-IgE milk allergies is that they’re often non-fatal. Overall, these distinctions between both reactions help researchers develop better diagnosis and treatment methods.
Milk Allergy Diagnosis

An allergist diagnoses a milk allergy through various tests targeting their patients’ symptoms. One way an individual can be diagnosed is by taking a blood test, where small blood samples are taken from one’s arm. Afterward, these samples and milk proteins are mixed in a lab so the allergist can measure the levels of IgE antibodies. It usually takes nearly a week before an individual gets their results back.
Secondly, a skin prick test has one’s skin exposed to milk proteins in small amounts where controls are applied to the skin to test and compare allergic reactions. If the control is positive, it has a histamine solution causing a raised, itchy bump to develop on the skin, spanning a few minutes. On the other hand, a saline solution is in a negative control and usually causes no response. Alternatively, an allergist may use a graded oral challenge to get a definitive diagnosis. This method requires an individual to ingest small sips of milk while observed for a reaction and tends to last around four hours.
Babies and Young Children
Babies at risk of developing a milk allergy may benefit the most from breastfeeding or taking hypoallergenic formulas. It’s recommended that high-risk infants stay breastfed for as long as possible. To avoid development, mothers should consider excluding milk from their diets to protect their children from allergens.
In contrast, hypoallergenic formulas offer alternatives as they can break down and process enzymes. These formulas can be either hydrolyzed, partially or entirely, or elemental, however, the ones consisting of amino acids are less likely to trigger allergic reactions. Specifically, soy-based formulas are another healthy option but can potentially cause soy allergies.
Final Thoughts
Although preventing a milk allergy from developing remains challenging, avoiding certain foods may stop reactions. In this case, staying away from milk and other milk products is the best way to avoid becoming allergic. To be safe, read food labels carefully and be mindful of trigger foods including casein, whey, and even non-dairy products such as sausage and canned tuna.
One should even avoid milk-free products as well as they may hide milk proteins within them. For severe reactions, at-risk individuals should consult their healthcare provider about using or carrying emergency epinephrine. Moreover, wearing medical alert jewelry can benefit those who’ve already experienced these severe reactions.
Disclaimer: This article is intended simply to provide information. It does not replace the medical advice of a physician or other medical professional. Please speak with your doctor or therapist if you have any questions or concerns.