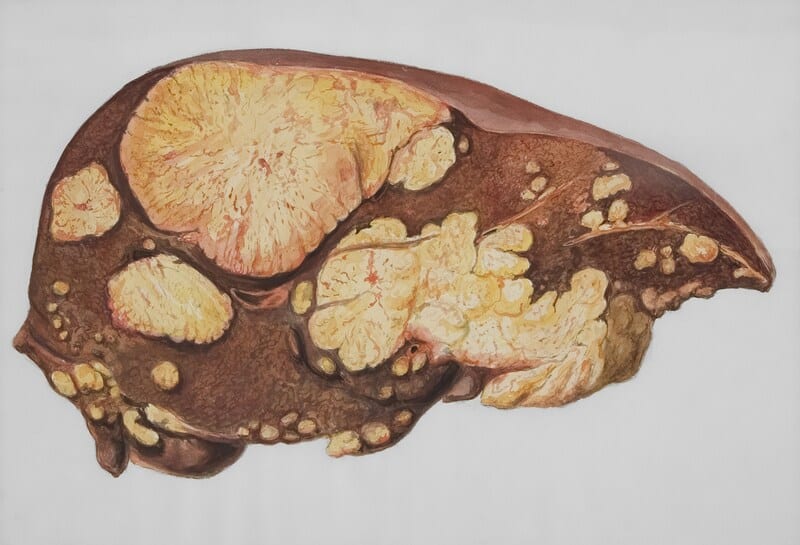
A person with cirrhosis of the liver deals with a severe health condition where damage impairs its function. Due to this chronic disease, one may risk developing liver failure in the future. Typically, prolonged liver damage causes this condition to emerge as the liver accumulates damage over the years.
Understanding Cirrhosis of the Liver
This late-stage liver disease gradually replaces healthy liver tissue with scarred ones. Most researchers suggest chronic hepatitis is to blame for cirrhosis of the liver as it causes inflammation in the tissues. To be precise, hepatitis A overstimulates the liver’s repairing process by causing this inflammation. While the liver repairs itself, scarring occurs, creating an accumulation of scar tissue that damages the liver, further hindering its ability to function correctly. Due to this damage, the liver gradually deteriorates, resulting in an inability to complete important tasks. If left unchecked, an individual may develop chronic liver failure, which is considered the final stage of liver disease.
Compensated and Decompensated Symptoms
Cirrhosis of the liver is characterized as a progressive condition where scar tissue accumulates, causing severe liver damage. While the body can adapt to compensate for the worsening liver function, it can also mask symptoms in a phase called compensated cirrhosis. However, noticeable symptoms will begin to emerge as the liver continues to weaken, signifying its transition to the next phase: decompensated cirrhosis.
As scarring increases and intensifies, the pathways where oxygen and blood flow through the liver gradually become blocked. This obstruction slows the liver’s ability to process nutrient metabolism, toxins, and blood. Likewise, it also impairs its essential protein synthesis and bile production. Moreover, the compression of scar tissue of important blood vessels can cause portal hypertension.
Declining Liver Function Symptoms

Although cirrhosis of the liver is a global health concern, middle-aged individuals are the most likely to develop it. Surprisingly, this condition is relatively common in the U.S., impacting nearly 0.25% of adults, with 0.50% being individuals between 45 and 54 years old. Alarmingly, this liver disease is responsible for around 26,000 deaths per year nationwide.
Depending on the disease’s advancement, symptoms of cirrhosis in the liver can vary, either being present or remaining invisible. Furthermore, early symptoms may include loss of appetite, malaise, upper abdominal pain, palmer erythema, fatigue, nausea, and spider angiomas. Specifically, cirrhosis’ advancement eventually causes numerous symptoms to emerge and are separated into two distinct groups: declining liver function and portal hypertension.
Declining liver function has numerous symptoms, including jaundice, dark urine, digestive issues, weight or muscle loss, pruritus, hepatic encephalopathy, and much more. For men and those assigned male at birth, in particular, enlarged breasts or shrunken testes are common symptoms. In contrast, symptoms of portal hypertension tend to be more severe. Its symptoms include abdominal swelling (ascites), fragile skin (coagulopathy), edina, breathing difficulties, blood in stool, and low urine output.
Risk Factors
Since cirrhosis of the liver is triggered by inflammation, any chronic disease leading to the development of chronic hepatitis can cause it. While alcohol-induced hepatitis forms as a result of consuming heavy alcohol, non-alcohol-related steatohepatitis is caused by excess fat stored in the liver. Comparatively, the viral infection, chronic hepatitis C, can be cured with antivirals. Although chronic hepatitis B has no cure, it can still be treated.
Autoimmune biliary diseases, including primary biliary cholangitis and autoimmune hepatitis, are less common causes. Other less common causes are genetic disorders such as Wilson Disease and Glycogen storage disease. Moreover, medication use, like over-the-counter medications and environmental toxins, can contribute as well. Even cardiovascular conditions such as chronic ischemia and congestive heart failure can cause cirrhosis of the liver to develop.
Cirrhosis and Portal Hypertension
Both cirrhosis of the liver and portal hypertension have various symptoms ranging from debilitating to life-threatening. In the beginning, mild symptoms of fatigue, general toxicity, reduced immunity, and mental fogginess emerge before other symptoms occur and exacerbate the condition. These additional symptoms include hormonal imbalances, fluid swelling or leakage, digestive issues, malnutrition, and malabsorption.
What’s more? An individual with cirrhosis of the liver may develop motor dysfunction or mild cognitive impairment. However, they can deal with more severe complications such as spontaneous bacterial peritonitis, and respiratory and kidney failure. Due to prolonged cirrhosis, one has a higher risk of developing life-threatening diseases such as liver cancer and chronic liver failure.
Final Thoughts
Early intervention is widely considered to be the best way to prevent liver diseases from becoming cirrhosis. However, early detection remains challenging as symptoms remain invisible in the beginning stages. Therefore, routine checkups are important for the best possible diagnosis shot. With early intervention, an individual can make life changes or seek treatment before the liver damage is irreversible.
Disclaimer: This article is intended simply to provide information. It does not replace the medical advice of a physician or other medical professional. Please speak with your doctor or therapist if you have any questions or concerns.